Staffing Changes at Central Washington Hospital Have Nurses Sounding the Alarm
Confluence Health made changes some nurses say lower the quality of care, increase likelihood of burnout among a workforce already stretched thin

It’s no secret there’s a nationwide shortage of nurses.
It’s a trend affecting Washingtonians too, including folks in North Central Washington who rely on medical care provided by Confluence Health. Confluence Health, which owns and operates Central Washington Hospital in Wenatchee, provides medical care some patients travel 100 miles or more to access. It’s a labor issue that’s led hospital administrators here and across the country to try to find ways to do more with less.
In December 2022, administrators at Confluence proposed changes to staffing policies that provide guidance on the nurse-to-patient ratio at Central Washington Hospital.
Those changes went into effect and a representative of the local chapter of the Washington State Nurses Association says it’s lowered the quality of care patients have come to expect from Confluence and will lead to increased burnout – further exacerbating the problem of staffing shortages in the healthcare industry.
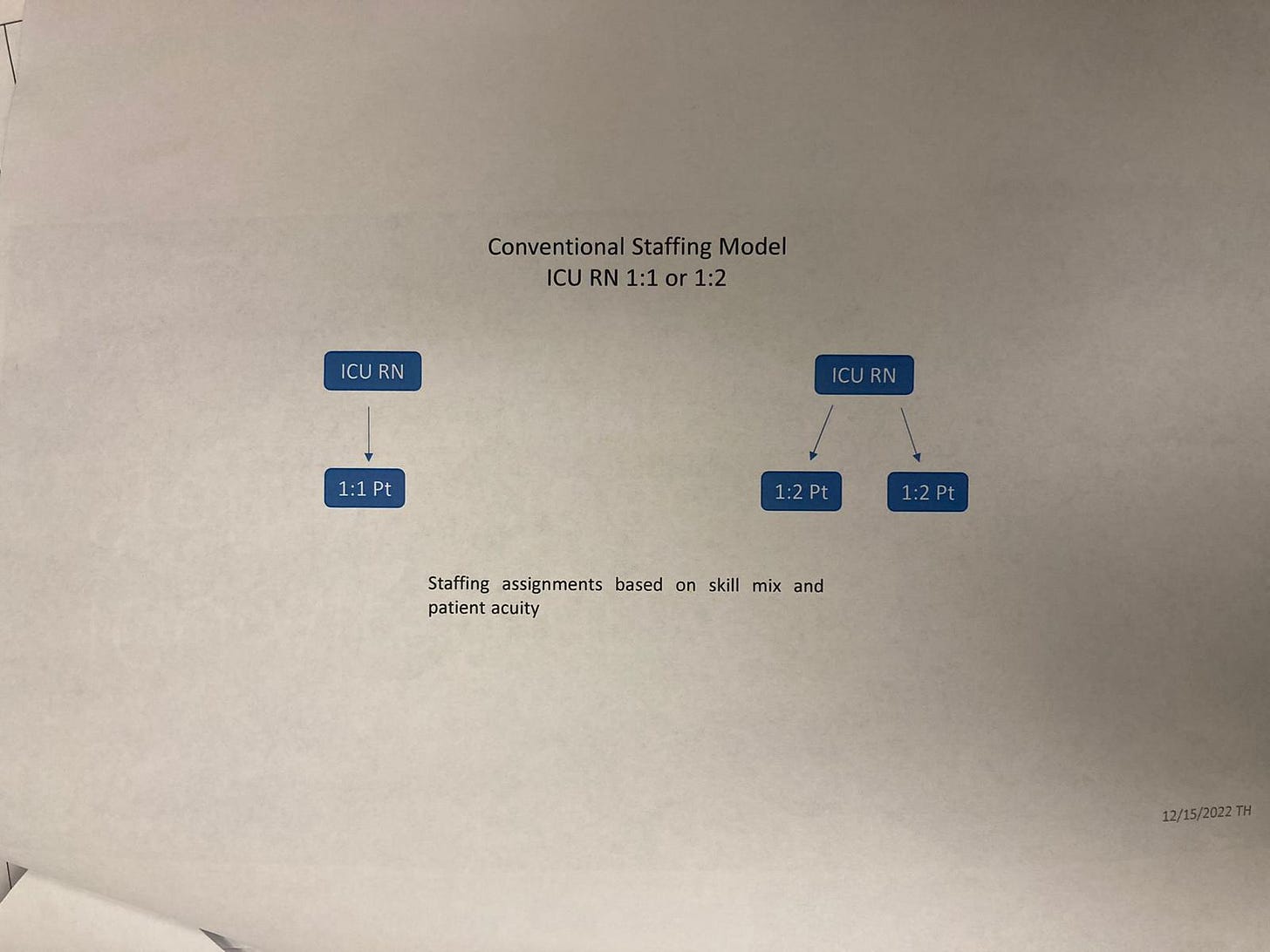
For example, in the Intensive Care Unit the nurse-to-patient ratio is usually one-to-one or one-to-two.
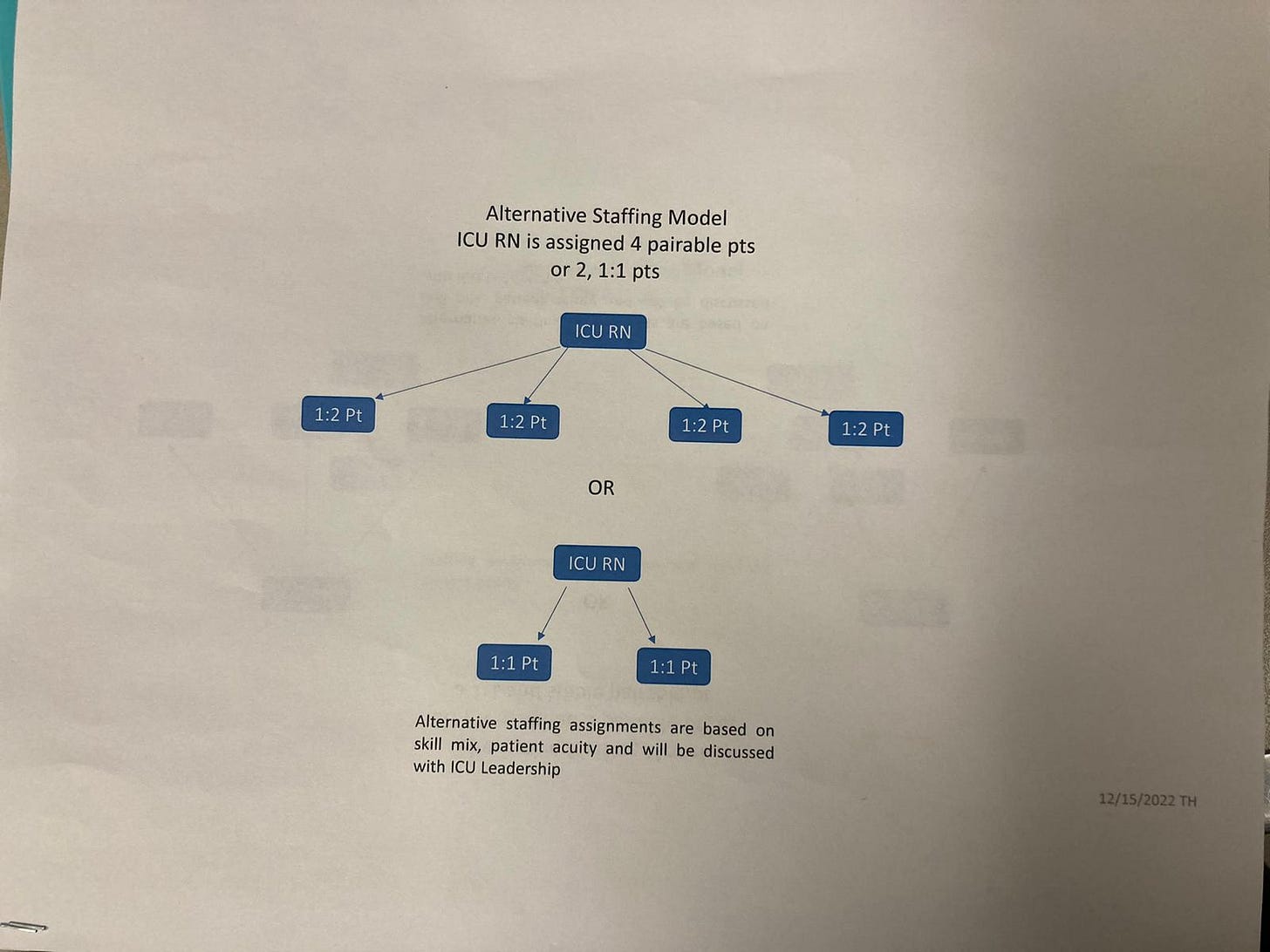
But according to documents posted by administrators in December, that policy would change to potentially one nurse per four ICU patients – depending on the circumstances and needs of those patients.
Sara Bergenholtz, chair of the local chapter of the nurses’ union, said the changes will not only lead to higher rates of burnout among already overworked nurses, but it has increased wait times for patients and led to fewer beds available in critical areas like the Emergency Room.
Adam MacDonald, a spokesperson for Confluence Health, says the staffing plan is consistent with national recommendations put forth by the American Nursing Association and Confluence currently has adequate staff to meet patient needs, although they are hiring and are not immune to national trends.
I reached out to both the nurses’ union and Confluence Health to ask about the changes and how they impact staff members, as well as patients, and below I provide my questions and Bergenholtz and MacDonald’s answers in a lightly-edited format.
Before we get to that though, I want to provide some context on how this story fits into statewide and national trends.
According to Politico, hospital administrators nationwide say worker shortages are their biggest concern. In Washington, a Feb. 2023 poll of state healthcare workers reported that “half say they are likely to leave the healthcare profession in the next few years” and 80 percent report feeling burned out by their jobs. Nearly half of the healthcare workers polled reported feeling unsafe at their jobs and, “short-staffing and workplace safety are among the top reasons healthcare workers are considering leaving the healthcare profession.”
There’s currently a bill being debated in Olympia that if passed would regulate the number of patients each nurse could be assigned. That proposed legislation has been covered by statewide media outlets already and, until recently, the state nurses’ union and the Washington State Hospitals Association have found themselves on opposite sides of the issue. However, according to the Hospitals Association, the two sides reached a compromise on the bill at the end of February.
That legislation is something to keep an eye on. But the main question right now is: how are these nationwide trends affecting nurses and patients right here in North Central Washington?
That’s what I aimed to find out when I reached out to both the nurses’ union and Confluence Health recently.
Here are my questions to union rep. Sara Bergenholtz and then Confluence Health spokesperson Adam MacDonald, who worked with Confluence’s chief nursing officer Kelly Allen to respond to my questions. Confluence’s responses are attributed to MacDonald.
A quick note on the length of the responses and why I decided to not edit them down: Bergenholtz’s answers are longer. I didn’t edit them down because I want to be fully transparent and not lose any context by truncating answers. Additionally, in this format articles can go longer than the average print piece so I decided to leave them. The length of Bergenhltoz’s answers in no way implies support for her point of view.
Here’s what they had to say:
Q: What brought about this change in staffing?
Bergenholtz: “Unfortunately, the change in tone and direction of the nurse staffing committee and the staffing plan appear to be the result of financial concerns and the newly born desire to have CWH follow “the industry standard” for nurse staffing. An industry standard is a difficult standard to pin down, as there is a wide variation on nurse-to-patient assignments across the country. In Florida, a nurse can expect to work with eight patients on a single shift, for a time, in New York, nurses were caring for up to 12 people at a time. Last year, this would have been considered “crisis staffing” for CWH. Generally, it is not uncommon to see a medical-surgical nurse taking anywhere from five to eight patients depending on the shift, state and company they are working for. Which is exactly the problem. We know, from decades of research, that a person’s risk for mortality increases by 7%-10% for every extra person assigned to their nurse and the best outcomes are seen with assignments of four patients or less. Yet there is no consistent standard, even within the same city, outside of California where they have laws that dictate minimum staffing numbers.
Unlike many other facilities, before this fall CWH had always followed evidence-based recommendations for nurse staffing, and we had some of the best, and safest nurse-to-patient staffing in the country. Our previous staffing levels were considered the gold standard for nurses and safety, and those floors on which the staffing was decreased, nurses are now being asked to work under what used to be our contingency and crisis staffing levels. It is baffling to us that we were largely able to maintain our previous safe staffing levels throughout the pandemic and yet, now, when the state of emergency has been lifted, we are told that this is no longer an option.
This change is particularly difficult as many of the nurses now working at CWH remained in Wenatchee throughout all of the pandemic, declining to pursue the once-in-a lifetime travel wages being offered to remain at a facility were safe staffing was a priority and input from nurses was sought and valued. This change is also off-putting to those travel nurses who agreed to become permanent staff at CWH, as it was the previous staffing and culture surrounding nursing that led to their decisions to stay.
The changes in this practice, more common in the Midwest and further eastward, are often cited as issues these nurses were trying to escape.”
Q: Same question, and is CWH short-staffed?
MacDonald: “Confluence Health is not immune from the current national staffing crisis in healthcare. The American Hospital Association (AHA) released the 2022 Q3 Health Care Jobs Report for our Region (Region 9) that shows Washington is second to California with open nursing positions with 4,900 openings. We are currently hiring for medical positions – RNs, CNAs, MA-Cs – and would like to increase the number of staff to help expand the care options and service we can provide. While we would like to increase the number of staff and are actively hiring, this does not mean Confluence Health is short-staffed. Confluence Health currently has enough staff to meet patient needs, though, as stated, we are looking to hire more to help expand care options and service.”
Q: Will these changes result in a higher rate of burnout among nurses?
Bergenholtz: “We are deeply concerned that, as decades of evidence-based research has shown, this will increase the rate at which the remaining nurses burn out and leave the profession as they are unable to provide safe or quality care.
Hospitals and their administrators across the country have proven that they cannot be left alone to prioritize the safety of those who use their services, something that is particularly true in rural areas where there isn’t any real option for where you’ll go for care.
If you’re having a stroke or need a cardiac surgery, you’re going to come to CWH because there isn’t anywhere else within 100 miles to go. And right now, that means that after a brain surgery, you may well be in the care of someone who has the responsibility of caring for two or three other people when the accepted standard is one-to-two at most.
Without the assistance of a certified nursing aide, and a charge nurse who is expected to take on secretarial duties since the removal of the unit clerk from their staffing, a nurse doesn’t have support. This isn’t sustainable and the last few years has shown us that nurses simply won’t sustain it. They’ll leave and things will only get worse.”
Q: Same question, and what is considered "the industry standard of care?"
MacDonald: “Our staff at Confluence Health are our most valuable resource and all efforts are made to ensure that Confluence Health provides not only industry-leading care but is also a great place to work. While patient care is always our foremost priority, we cannot succeed in this area without our outstanding staff and providers so all decisions are always made with an eye for maintaining or even increasing workplace satisfaction.
As there are no federal standards set for nursing ratios, the phrase “industry standard of care” is a bit ambiguous. The American Nursing Association (ANA) has recommendations for safe staffing which Central Washington Hospital uses in its nurse staffing committee.”
Q: What does this change mean for patient care?
Bergenholtz: “We had hoped that the closing of one of the hospitals step-down units (PC1) in November indicated a desire to protect patients and staff by maintaining our previous ratios. Such an effort would not have been beyond what we had previously experienced with our leadership, yet instead we saw this further exacerbate the situation. The closing of this unit appeared to be an effort to decrease the use of travel nurses and to make the changes to our staffing more workable. In addition to the reduction of services, this has led to increased wait times. There are fewer available beds in the hospital now, and those who have been admitted can spend more than 24 hours in the emergency room waiting for a bed/room to become available.
In an emergency room that only has 25 beds, when 20 of them are occupied for a day or longer there isn’t any option beyond making the people who come to the ER wait to be seen. There isn’t anything the staff, no matter what license they hold, can do to change it.”
Q: Can patients expect a lower quality of care because of these changes? Have these changes resulted in longer wait times for patients?
MacDonald: “Confluence Health prides itself on always providing industry-leading care and makes all changes with patients and their care in mind. While during December 2022 our emergency and walk-in departments did experience longer-than-normal wait times due to the sharp nationwide increase in cases of respiratory and seasonal illnesses, which was announced in a press release, this was not due to staffing but to the increased demand seen not only in North Central Washington but statewide and indeed across the United States. Since that time, wait times have returned to more typical levels.”
Q: Did Confluence take into account any of the input from the union before making this decision?
Bergenholtz: “The union made no specific recommendations for the staffing plan, although the nurses on several units engaged with their nursing leadership to develop plans that were both cost-effective and safe. These plans were never presented to the Nurse Staffing Committee as those above the nursing leadership decided they did not go far enough prior to them being presented. At the last staffing committee meeting in December, Staff Nurse Representatives specifically stated that they wanted to discuss the proposed changes with colleagues on those units most affected before voting. The plan was approved by our CEO without that follow-up having occurred.”
Q: The nurses' union says its policy proposals regarding staffing were rejected by Confluence and they didn't have adequate input in the policy CEO Andrew Jones proposed prior to it being implemented. Was the nurses’ staffing committee consulted or given input on the changes before they were implemented?
MacDonald: “Confluence Health has a robust nurse staffing committee, which is a result of the Patient Safety Act passed in 2017. All changes made to the staffing plan go through this committee for feedback and input. Confluence Health follows the process outline in the RCW for how we are able to change and submit our staffing plan to the Department of Health.”
Q: I understand this is a state and even nationwide problem, but what do you think is the best way forward to ensure adequate staffing in our medical facilities in this region?
Bergenholtz: “Staffing committees were supposed to be a compromise to ensure that those providing care to people had a voice and the ability to influence staffing, but they have proven to be no more effective in ensuring that people are valued over profits than any other effort.
We are not alone in having our voices ignored in the development of a staffing plan, it’s just less tolerable to us because it is a situation that has not previously occurred at CWH. The answer, the only answer left to us, is mandatory ratios that put in place a minimum staffing level. Such a change would remove the ability of the CEO to veto safe staffing plans in favor of profits and end the nationwide practice of short-staffing nurses to increase profit.
The hospitals and their representatives, particularly the Washington State Hospital Association, will tell you that they can’t staff the beds they have, that this will result in a decrease in services. It’s what they always say, it’s what they would say to anyone who would listen last year when it looked like a staffing bill might actually be passed. Yet everything they claimed would happen as a negative and inevitable consequence of mandatory ratios is happening any way, and nurses are continuing to flee the bedside because they refuse to pile trauma on top of trauma and work in conditions that we know will end in preventable harm and death.
Across the nation, hospitals wail and whine about not having enough nurses, about losing money to travelers to replace them, but they never come to the table with any answers. They never present a new idea, an innovative change to a system that serves them, and exactly no one else, well. They continue to do the same thing over and over again, continue to fall back to the behaviors and actions that caused this situation in the first place. At our final staffing committee meeting the question was asked, “How is doing the exact same thing that got us into this situation supposed to make it better?” No one had an answer. As the hospital representatives on our staffing committee are also nurse leaders, I like to think that they agreed with us.
Another issue that needs to be looked at in this, and other states, is reimbursements. Medicare and Medicaid have no issue with leveling financial penalties against a hospital, yet the rate of reimbursement they provide is often cents on the dollar, exacerbating an already tenuous situation. The failure of our federal and state legislatures to address this is a failure of the responsibilities of government at its most basic levels. Ensuring those who qualify for benefits are actually able to get care without burdening the system should be seen as integral to the role of government as ensuring the roads are maintained and the mail is delivered.
In the United States, Medicare only provides limited long-term and hospital benefits, so those dependent upon this service are often supplemented by Medicaid. It is Medicaid that pays for memory care and extended hospital stays, and it is Medicaid that is currently reimbursing hospitals at a rate that is less than ten cents on the dollar. It’s easy for us to demonize hospitals and their administration, but we have chosen a capitalist system and the realities of that system require adequate reimbursement. Medicaid’s failure to increase its reimbursement rates has resulted in the elderly and disabled spending months in hospitals, remaining there long after they actually need the care provided in an emergent or acute-care setting and resulting in an increased rate of decline. Facilities that specialize in the care of these populations cannot pay their own bills when the majority of their patients are on Medicaid, so they limit the number of Medicaid recipients that they take. This results in desperate families bringing their vulnerable family members to the emergency room, trusting that the system will find a way to provide care for them.
We can’t fix the nursing shortage by pretending the need for hospitals to receive adequate reimbursement is a separate issue. We have no desire to see the smaller, local, hospital systems fail under ever increasing financial burdens. Those of us not disabled, or caring for the disabled, are blessed to not be put in such a difficult situation. But we are all going to age. We are all going to need some kind of care as we age, and if only for the preservation of our own interests, we need to see this issue addressed. Failure to do so will only result in the loss of access to medical care, regardless of how we choose to address nurse staffing.
The Washington State Legislature is currently reviewing bills and requests on these issues. Senate Bill 5236 would direct L&I to establish minimum safe-staffing assignments, and there is a hard push to increase Medicare reimbursements and facilitate the discharge of hard-to-place patients into safe and appropriate settings. Each effort is important and each holds a piece to the puzzle of protecting healthcare in Washington state. Each of these issues needs the support of Washington citizens during this legislative session.
This isn’t a union and hospital issue. This isn’t a physician or a nurse issue. This is an issue that stretches through every community into each of our households, and it is my hope that we will be able to see positive developments through the support of the people of Washington state.”
Q: SB 5236, a new bill in Olympia concerning hospital staffing, has the nurses’ union support. The state hospitals association is against it. What is Confluence Health's position, and is there anything else you think the public should know about this issue?
MacDonald: “Confluence Health has been informed that the nursing unions and the Washington State Hospital Association (WSHA) have come to an agreement on an amended version of this bill that better addresses the nursing shortage while keeping the quality of care for the patient front and center of focus. The press release for this announcement is available here.
Due to the nature of illness and medical needs, staffing is always an area that requires updating, discussion, and changes to continue to provide the best in care to patients. As COVID-19 demonstrated, healthcare facilities, including Confluence Health, constantly strive to adapt, update, and respond to patient needs to ensure that this excellent care continues. We are proud each and every day of the amazing work being performed by our dedicated, professional, and caring staff and providers for the residents of North Central Washington. We are also thankful to our communities for the trust they place in us and are grateful that we get to play a role in their health. It is our steadfast goal to continue providing that excellent care and to be worthy of the trust placed in us.”
The Covid Vaccine Mandate Issue
Nurses like Kirsten Jerezano and the plaintiffs in the lawsuit against Confluence Health over Covid-19 vaccine mandates would have folks believe the nationwide nursing shortage is because of Covid vaccines. And while it’s a problem that was undoubtedly accelerated because of Covid-19 and various responses to it – the nationwide shortage of nurses was an issue that predates the pandemic.
I followed up with MacDonald to ask if Confluence Health’s Covid vaccine mandate is a contributing factor to any staffing issues they might be having, and will update this piece once I hear back.
Update as of March 8: Confluence Health does not have any comment on this issue.
My Two Cents
All four of my children were born at Central Washington Hospital. During the birth of our youngest child, less than two years ago, my wife passed out and the baby’s heart rate dropped. I was sitting by my wife’s bedside and jumped to my feet as alarms sounded. I was powerless to do anything but knew something was seriously wrong. Before I made it to the door nurses burst into the room and went to work. I looked on, light-headed – heart in throat.
Five nurses surrounded her bedside, each focused on important and complicated tasks while calling for backup. Before any could arrive, she had come to and the baby’s heart rate had stabilized. Doctors weren’t far behind, but those nurses were there immediately and made a big difference. In the end, my wife gave birth (after 18 hours in labor) and we welcomed to the world a baby girl we named Olivia. She is one of the lights of my life, and I couldn’t imagine my life without her – or my wife or other children.
I include this memory because I, as well as my whole family, have and will most likely be Confluence Health patients in the future.
Part of this issue is economics – supply in demand. There aren’t enough well-trained nurses to go around.
Part of this issue is labor versus capital. Again, economics.
The bottom line is there’s no story without patients – people like you and me. Healthcare is an industry and we are the customers. Without us, there’s no industry and thus, no jobs. Economics.
If you, like me, are a customer of the healthcare industry, then I suggest you pay attention to the progress of SB 5236. I certainly will be and will follow up on the state of healthcare in North Central Washington in the future.




Dominick- Thank you for your insightful and factual articles. What’s the best way to submit to you ideas for coverage of other local stories that might be of interest to your subscribers and the general public?
McDonald says, “ We are hiring for medical positions, RNs, CNAs.” These are NURSING positions and his language tells the tale of the problem. The history of Confluence’s collegial relationship and their nursing professionals is gone with the new leadership. Nursing is its own healthcare science. McDonald also repeatedly speaks of his industry. Medicare is one of the few remaining large chunks of money in America available for plunder. Pharma and the health insurance INDUSTRY are accountable for our disgraceful healthcare outcomes in America. Nothing will change until we get the INDUSTRY out of healthcare. When I read about the treatment of nursing leadership at CWH by the new administration, I came to the conclusion, as a 45 year RN, that if I or my husband need major surgery, we will go to UW Medicine in Seattle or Spokane (I for sure don’t trust the Catholic hospitals, they are the worst money grubbers , denying charity care to their patients until they were sued TWICE by AG Ferguson.). Thanks, again, Dominick, for covering an important story like no one else.